Written by Dr Gabriel Scripcaru and Dr Predrag Nikolic
Recognising the defining clinical features of various types of skin cancer, and an appropriate approach to the biopsy, are essential for their diagnosis and management. The importance of a timely diagnosis cannot be overemphasised, in view of achieving the best possible outcome and minimising the complications.
This article aims to discuss squamous cell carcinoma (SCC) and basal cell carcinoma (BCC), two of the most common cancers Basal cell carcinoma (BCC) in Australia.
Patient skin history
It is important to record the relevant patient skin history prior to completing a full body skin check or examining a particularly concerning new or changing lesion, including:
- Family history of skin cancers
- Previous skin cancers
- Previous excisions
- Occupation
- Past UV exposure/sunburn including use of solariums
- Frequency of sun protection
Squamous cell carcinoma (SCC)
 |
 |
| Clinical Features | Histology |
SCC is a malignant epithelial tumour of keratinocytes arising most commonly in sun-damaged skin. The vast majority of cases are associated with pre-existing actinic (solar) keratosis, squamous cell carcinoma in situ, or both. SCCs account for nearly 30% of non-melanoma skin cancers.
Some SCCs may be associated with human papillomavirus, chronic inflammation or radiation therapy.
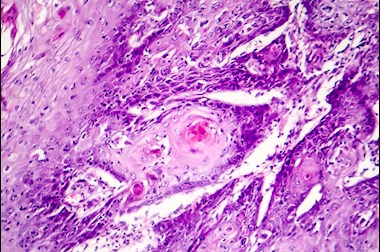
From a histological point of view, these lesions may be well differentiated, moderately differentiated or poorly differentiated. The degree of differentiation is an essential marker of progression, risk of metastasis and prognosis. Many lesions display areas of varying degrees of differentiation, however, the worst area is to be considered when finally grading the lesion. It is the least differentiated area that ultimately determines the management and prognosis.
SCC with focal basaloid differentiation or basosquamous carcinoma, is regarded as a moderately differentiated lesion. Poorly differentiated SCCs are characterised by the absence of keratinisation. SCC may be slow or fast growing. In some cases, significant clinical changes may be evident within months, or even weeks.
Clinical features
- Thickened red, scaly spot
- Slowly or rapidly growing papule or nodule
- Non-healing ulcers or recurrently bleeding
- May be tender to touch
- May be pigmented, raising the clinical suspicion of a pigmented lesion
High-risk features
- SCCs found on the head and neck are considered high-risk
- Occurrence in immunosuppressed patients or at sites of previous pathology or trauma (e.g. burn scars, radiation scars, chronic ulcers/sinuses)
- The tumour growth is rapid, has a diameter >20mm, poorly defined margins, field change, fixed to underlying structures, located over important structures or numerous tumours
- The patient experiences symptoms that suggest perineural invasion (e.g. tingling, pain, paraesthesia, formication, dysesthesia or impaired motor function)
- Where a biopsy has been performed, high-risk histopathological features include: tumour thickness >6 mm, invasion beyond the subcutis, lymphovascular invasion or high-risk pattern of perineural invasion, poorly differentiated tumours and/or aggressive subtypes (e.g. infiltrative/desmoplastic, sarcomatoid)
Basal cell carcinoma (BCC)
 |
 |
| Clinical Features | Histology |
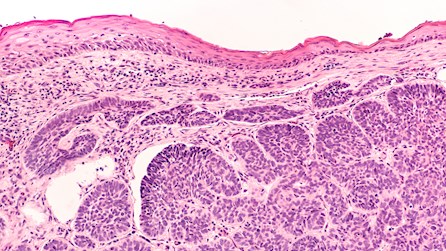
Basal cell carcinoma (BCC) is a slow-growing locally invasive tumour, arising most commonly in sun-damaged skin from the basal layer of the epidermis. Progression of disease usually takes the form of local tissue destruction, but rarely progresses to metastases.
Histologically, tumours display several architectural patterns: nodular, superficial (which may represent an early phase of a nodular pattern), superficial multifocal, infiltrative, micronodular, morphoeic and metatypical (i.e. squamous or sebaceous differentiation). Often, a mixed pattern is observed in the same lesion.
Patient-related factors and the presence of high-risk features determine the course of treatment. BCC is the most common cancer in humans and accounts for nearly 70% of non-melanoma skin cancers.
Clinical features
- Pearly, translucent papule, plaque or nodule
- Scaly, dry area, shiny and pale or bright pink in colour
- Recurrent bleeding or ulceration
- May be pigmented, raising the clinical suspicion of a pigmented lesion
High-risk features
- Head and neck BCCs >10 mm are considered to be high-risk tumours
- Trunk and extremities BCCs >20 mm are considered to be high-risk tumours
- Aggressive histologic subtypes (e.g. micronodular, infiltrative, morphoeic or basosquamous/metatypical)
- Symptoms indicating perineural invasion (e.g. tingling, pain, paraesthesia, formication, dysesthesia impaired motor function)
- Fixation to underlying structures
- Genetic disposition of the patient (e.g. Gorlin syndrome or Xeroderma pigmentosum) and use of immunosuppressants
Steps prior to removing SCC/BCC
Prior to the excision of the tumour, the diameter should be measured and recorded. Tumour measurement after excision is not accurate due to tissue shrinkage, which occurs after excision and during specimen fixing and processing. The plane of section examined histologically is relevant to the distance from the tumour to the nearest margin, hence, it does not necessarily represent the greatest tumour dimension.
Confirming the diagnosis and notes on the histology report
In the first instance, the surgical options include a shave or punch biopsy for diagnostic purposes, or complete curative excision without prior tissue diagnosis. Primary curative excision is usually undertaken in cases of high clinical suspicion or at the patient’s request.
A punch biopsy has the advantage of including the deeper aspect of the lesion and is easily processed with a lower risk of tissue artefacts.
Depending on its size, a shave biopsy may better reveal the architectural pattern and it may include a larger portion of the lesion, however, it may not include the deeper aspect of the tumour and it may be prone to artefacts, if it is too thin. A thicker shave is preferred to avoid folding or fragmentation which could significantly impair the histological assessment. A thicker shave biopsy also provides better insight into the tumour depth and architecture. It is important to note that margins cannot be accurately assessed in a punch or shave biopsy, although small lesions may be often completely excised employing one of these biopsy types. The presence of clear edges may be mentioned in such cases in the histological report, however clinical correlation is essential when determining the need for further excision.
Surgical excision is the treatment of choice for both SCC and BCC
There is no clear evidence-based recommendation regarding the minimum excision margin. Factors such as risk status of the tumour, surgical accessibility, patient age, co-morbidities and wound-healing capacity should be considered when deciding on the excision margin.
Clinical guidelines are regularly communicated and updated in publications and at conferences. Regardless of the guidelines followed by the clinician, it is important to note, that due to tissue shrinkage, the reported histological margins may be as little as half of the clinical margin measured at the time of surgery.
The histological report indicates the clearance of margins in the planes of section examined rather than representing an absolute guarantee of complete excision of the tumour. Re-excision, with the same recommended clinical margins as in the initial excision, should be attempted when involved margins are reported.
In approximately 50% of cases where a tumour was present at the edges of the biopsy, or at the margins of the excision in the initial specimen, there will be no further residual tumour in the re-excised specimen. This is explained by the fact that a minimal amount of residual tumour at the edge of the initial biopsy has been eradicated by the immune response and the regenerative process leading to repair and scarring following the initial surgical intervention.
Additional aspects of management
In cases of SCC with perineural invasion (PNI) or lymphovascular invasion (LVI), the patient should be referred to a specialist (radiation oncologist or hospital skin cancer unit). In cases of LVI, further investigations in view of staging may be indicated, while in cases of PNI, adjuvant therapy, such as radiation therapy may be employed.
Non-surgical options for BCC
Unlike in cases of SCCs, non-surgical options exist for a subset of BCCs. Cryotherapy, curettage and cautery can be used in combination in patients who cannot tolerate surgery. BCC rarely presents with LVI. Those cases should be treated like a moderately differentiated SCC with LVI. PNI is a more frequent occurrence in high-risk BCC. Radiation therapy may be indicated in these cases and the patient should therefore be referred to a specialist (radiation oncologist or hospital skin cancer unit) for further staging and management. Superficial BCC can be managed using a non-surgical approach.
Other treatment options, reserved for superficial BCC, include topical therapy such as Imiquimod (Aldara) cream and topical photodynamic therapy. These methods are generally not suitable for cases of BCC with high-risk features.
About the authors

Dr Gabriel Scripcaru
Qualifications: FRCPA, MD
Lab: Clayton, Vic
Areas Of Interest: Skin Pathology, Head, Neck & Soft Tissue Pathology
Speciality: Anatomical Pathology
Phone: 1300 134 111
Email: gabriel.scripcaru@clinicallabs.com.au
Dr Gabriel Scripcaru studied medicine at the University of Medicine and Pharmacy “Gr.T.Popa”, Iasi Romania. After graduation he commenced training in neurosurgery working in Cluj, Romania and Newcastle, England. He subsequently became a member of the Royal College of Surgeons of Edinburgh upon completion of the required examinations. Gabriel’s clinical experience prior to anatomical pathology also included working in emergency medicine, intensive care and surgery both in Australia and Scotland. His training in anatomical pathology comprised rotations at the The Royal Melbourne Hospital, The Royal Women’s and Royal Children’s Hospitals in Melbourne. Before joining Australian Clinical Labs, Dr Scripcaru worked at Southern Sun Pathology in Sydney where he gained experience in dermatopathology.

Dr Predrag Nikolic
Qualifications: MBChB, MMedSci, PhD, FRCPA
Lab: Clayton, Vic
Areas Of Interest: Lung Pathology, Breast Pathology, Skin Pathology, Molecular Diagnostics
Speciality: Anatomical Pathology
Phone: 1300 134 111
Email: predrag.nikolic@clinicallabs.com.au
Dr Nikolic is a consultant histopathologist with an interest in lung pathology, breast pathology, dermatopathology and molecular diagnostics. Dr Nikolic completed his undergraduate medical degree and his masters degree (immunopathology) in Belgrade, Serbia and subsequently moved to New Zealand where he obtained a PhD degree at the University of Auckland, working on purinergic signaling and programmed cell death. He worked as a lecturer and as a medical officer in Auckland and moved to Australia to train in anatomical pathology. He received his pathology training at Monash Medical Centre and at Healthscope (now Australian Clinical Labs) and obtained his FRCPA in 2011. On completion of his training he stayed at Australian Clinical Labs as a consultant.
Local pathologists near you
 Dr Carl Bulliard
Dr Carl Bulliard
Qualifications: BSc (Med), MBBS, Grad Dip Med (Clin Epid), FRCPA
Lab: Bella Vista, NSW
Areas Of Interest: Pathology of the Skin, Head & Neck and Eye, Registrar Training
Speciality: Anatomical Pathology
Phone: (02) 8887 9951
Email: carl.bulliard@clinicallabs.com.au
 Dr Irani Dissanayake
Dr Irani Dissanayake
Qualifications: MBBS, MD, FRCPA
Lab: Adelaide Airport, SA
Areas Of Interest: Gynaecological Pathology, Gastrointestinal Pathology
Speciality: Anatomical Pathology
Phone: (08) 8205 5641
Email: irani.dissanayake@clinicallabs.com.au
 Dr Jenny Grew
Dr Jenny Grew
Qualifications: MBChB, FRCPA, AFRACMA
Lab: Subiaco, WA
Areas Of Interest: Breast, Gastrointestinal, Gynaecological & Cutaneous Pathology, Cytology and Molecular Pathology
Speciality: Anatomical Pathology
Phone: 1300 367 674
Email: jenny.grew@clinicallabs.com.au