Inflammatory Skin Disorders: A practical approach to biopsy diagnosis
Written by Dr Jenny Grew.
As the weather warms up and we dispense with a few layers of clothing, it is suspicious lesions and malignancies that feature prominently in presentations of skin disorders to general practitioners. All the more reason to keep in mind that inflammatory skin conditions - the dermatoses - may present at any time.
In this article, some common and not-so-common dermatoses are discussed: how they may present clinically, their typical pathological changes, including the level of skin involved - which in turn informs the best approach to taking a biopsy.
For any biopsy of an inflammatory skin condition, the provision of clinical information is essential and should include:
- Description of the lesions: duration and appearance, age of the lesion and any prior treatment.
Consider submitting a clinical photograph to the lab along with the specimen. - Clinical differential diagnoses.
- Medical, including drug, history.
Let’s turn our attention to three of the more commonly encountered dermatoses, each of unknown aetiology.
LICHEN PLANUS

Clinical Features
- Typically presents in patients 30-60 years
- Violaceous, flat-topped papules, often polygonal, streaked with white lines.
- Occurs on flexor surfaces of wrists, thighs, genitalia, trunk.
- Oral lesions may occur (in up to 60%)
Histology
Lichenoid pattern:
- Band-like upper dermal inflammatory infiltrate.
- Apoptotic keratinocytes in epidermis.
- Hyperkeratosis and wedge-shaped hypergranulosis.
Approach to Biopsy
- Incisional biopsy to include superficial dermis
- Include a small amount of normal skin at advancing edge of lesion.
- Punch biopsy in the centre of a lesional area may be suitable.
GRANULOMA ANNULARE
Clinical Features
- Typically occurs in patients younger than 30 years.
- More common in women and patients with diabetes.
- Lesions occur on hands, feet, extensor limb surfaces.
- Classical lesion comprises small papules with an enlarging ring configuration.
Histology
- Granulomatous: necrobiotic/interstitial.
- Increased dermal mucin.
Approach to Biopsy
- Incisional biopsy at advancing edge, to include reticular dermis.
- Annular lesions may be unsuitable for punch biopsy.
DISCOID LUPUS ERYTHEMATOSUS

Clinical Features
- Peak onset in fourth decade, more commonly occurring in women.
- Wide distribution but classical lesions involve head and neck, including butterfly malar rash.
- Red, scaly, well-demarcated patches with follicular plugging.
- Photo-exacerbation may occur.
Histology
- Lichenoid reaction involving epidermis and epithelium of plugged follicles.
- Inflammation involves superficial and deep dermis.
- Direct immunofluorescence may be positive (lupus band test) but not required for diagnosis.
Approach to Biopsy
- Incisional biopsy to include superficial dermis
- Include a small amount of normal skin at advancing edge of lesion.
- Punch biopsy in the centre of a lesional area may be suitable.
Two Less Common Conditions are Grover Disease and Porokeratosis.
POROKERATOSIS
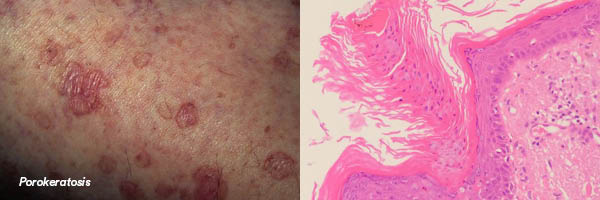
Clinical Features
- Various forms including familial (beginning in childhood), sporadic or associated with immunosuppression.
- May occur on sun-exposed sites (often legs) in middle aged adults as disseminated superficial actinic porokeratosis (DSAP). Lesions may be up to 10mm and resemble solar keratoses.
- Squamous cell carcinoma may develop (except in punctate form) indicating pre-malignant potential of porokeratosis.
Histology
- Cornoid lamella is the defining feature: a thin column of parakeratotic cells. Associated with focal loss of the granular layer and with vacuolated and dyskeratotic keratinocytes. Often a lichenoid reaction.
Approach to Biopsy
- Incisional biopsy at advancing edge, to include reticular dermis.
- Annular lesions may be unsuitable for punch biopsy.
GROVER DISEASE (TRANSIENT/PERSISTENT ACANTHOLYTIC DERMATOSIS)

Clinical Features
- Itchy grey-pink papules or papulovesicles, acute eruption.
- Precipitated by sweat, sun exposure, ionising radiation, some drugs.
- Typically occurs on trunk area of middle-aged and older Caucasian men.
- Transient and more persistent chronic forms.
Histology
- Tissue reaction pattern of “acantholytic dyskeratosis” with suprabasal clefting.
- Perivascular lymphohistiocytic infiltrate in superficial dermis.
- A few eosinophils may be present.
Approach to Biopsy
- The changes in Grover disease are superficial, so may be amenable to punch biopsy or shallow incisional biopsy. A solitary papule may be encompassed by a punch sample which ideally would include a surrounding rim of non-lesional skin.
Additional considerations:
Select an appropriate lesion (biopsy at different stages of a lesion according to clinical differential diagnosis):
- an early lesion in itchy or blistering conditions
- an lesion of intermediate duration if vasculitis is suspected
- a late lesion in lupus, psoriasis or fibrosing lesions
- avoid lesions which are ulcerated or have been treated, for example with topical steroids.
Is ancillary testing required?
- Infection: microbiology
- Blistering, vasculitis: direct immunofluorescence (DIF)
- Lymphoma: submit fresh tissue urgently to lab and/or in suitable transport media; discuss with dermatopathologist.
A further note on blistering conditions: samples should be submitted for histology and DIF. An intact blister should be submitted, usually necessitating a deep shave, incisional or excisional sample. The epidermis often becomes separated in a punch biopsy, rendering this an unsuitable technique.
Finally, clinicopathological correlation. Histological examination of a skin biopsy amounts to provision of a specialist medical opinion by a pathologist. Even in optimal circumstances, with clinical information to hand, appropriate biopsy technique and skilled lab processing of the sample, the consultation process can be greatly enhanced by collaboration with the reporting dermatopathologist. A phone conversation and discussion can go a long way to resolving a diagnostically challenging biopsy!
References:
1. Bolgnia JL, Schaffer JV, L Cerroni. Dermatology 4th edition. Elsevier, 2018.
2. Calonje E, Brenn T, Lazar A and McKee PH. McKee’s Pathology of the Skin, 4th
Edition. Saunders Elsevier, 2012.
3. Photo credits: DermnetNZ, Pathology Outlines, Prof Raimo Suhonen (Discoid Lupus
Erythematosus image)
4. Harvey NT, Chan J and Wood BA. Skin biopsy in the diagnosis of inflammatory skin
disease. Australian Family Physician, Vol 46, No. 5, May 2017.
5. Patterson JW. Weedon’s Skin Pathology, 4th Edition. Churchill Livingston
Elsevier, 2016