Placental Growth Factor (PlGF) for Early Onset Pre-Eclampsia (EO-PE) Screening
Written by Associate Professor Mirette Saad
As part of our Antenatal Screening offerings and in alignment with the new guidelines, Australian Clinical Labs is now offering Placental Growth Factor (PlGF 1-2-3™ assay-DELFIA Xpress®) blood test from PerkinElmer. Along with the combined First Trimester Screening (cFTS) and Harmony Non-Invasive Prenatal Testing (NIPT), PlGF is an additional first trimester screening marker. PlGF can be used to screen for Early-Onset Pre-Eclampsia (EO-PE) in pregnancy.
Pre-Eclampsia (PE)
Pre-Eclampsia (PE) is a multi-system disorder previously identified by the onset of hypertension accompanied by significant proteinuria after 20 weeks of gestation. In 2014, the definition of PE was broadened by the International Society for the Study of Hypertension in Pregnancy (ISSHP) (Table 1) and adopted by the Royal Australian and New Zealand College of Obstetricians and Gynaecologists (RANZCOG) 25 as it is considered a major cause of death and morbidity for the mother and perinatal death and long-term handicap for the baby. In the absence of proteinuria, the finding of maternal organ dysfunction is sufficient to make the diagnosis of PE 1.

International Society for the Study of Hypertension in Pregnancy (ISSHP) revised definition of PE, 2014
The revised ISSHP definition of pre-eclampsia (2014) is;
Hypertension developing after 20 weeks gestation and the coexistence of one or more of the following new onset conditions: |
|
1. Proteinuria
3. Uteroplacental dysfunction
|
Table 1: Quoted from Tranquilli AL et al. 2014 1
Pre-Eclampsia is a Spectrum Disorder 2,3,4
PE Can Be Sub-Classified Into:
- Early-Onset PE (with delivery at <34+0 weeks of gestation)
- Pre-Term PE (with delivery at <37+0 weeks of gestation)
- Late-Onset PE (with delivery at ≥34+0 weeks of gestation)
- Term PE (with delivery at ≥37+0 weeks of gestation)
These sub-classifications are not mutually exclusive. Early Onset PE (EO-PE) is associated with a much higher risk of short and long term maternal and perinatal morbidity and mortality 2,3,4.
Pre-Eclampsia is More Common than Aneuploidies 5,6,7,8
The prevalence of PE and related conditions (fetal growth-restriction and pre-term birth) is much higher than that of Down syndrome. PE affects 2-8% of pregnancies globally 7. The incidence is increasing with the global increase in maternal age, obesity and the use of assisted reproductive techniques. It also follows the rising incidence of diabetes, hypertension, and renal disease – all are known co-morbidities that predispose sufferers to PE during pregnancy.
Unlike Down syndrome, PE is a major cause of maternal and perinatal morbidity and mortality. Thus, preventing PE would bring substantial improvements to maternal and perinatal health 5,6,7,8.
Pre-Eclampsia and Early Assessment 9,10,11,12
Screening for PE can be performed at 11-13+6 weeks’ gestation by a combination of maternal demographic characteristics and medical history with some biophysical markers including mean arterial blood pressure (MAP) and the mean uterine artery pulsatility index (UTPI) along with measurements of biochemical markers 9,10,11,12. NHMRC recommend an assessment to all women for clinical risk factors for PE early in pregnancy 26.
Pre-Eclampsia (PE) Screening and New Guidelines FIGO Guidelines, 2019 4
In June 2019, the International Federation of Gynecology and Obstetricians (FIGO) released new guidelines to combat PE.
- FIGO adopts and supports the Fetal Medicine Foundation (FMF) position that all pregnant women should be screened for pre-term PE by the first-trimester combined test with maternal risk factors, MPAP, UTPI, and PlGF as a one-step procedure.
- FIGO adopts and supports the FMF position that in high-risk women, defined by the first-trimester combined test, aspirin ~150 mg/night should be commenced at 11–14+6 weeks of gestation until either 36 weeks of gestation, when delivery occurs, or when PE is diagnosed.
- FIGO encourages all countries and its member associations to adapt and promote strategies to improve access to prenatal services and encourage early booking.
- FIGO encourages all countries and its member associations to ensure that risk assessment and resource-appropriate testing for pre-term PE become an integral part of routine first-trimester evaluation protocol offered at all maternal health services.
Biochemical Markers in Pre-Eclampsia 9,10
Biochemical markers that reflect placental function, such as Placental Growth Factor (PlGF) and pregnancy associated plasma protein-A (PAPP-A), are significantly reduced in the first trimester, and throughout the pregnancy, in patients that will later present with pre-term PE with delivery <37 weeks’ gestation.
Of these two markers PlGF is a better PE screening marker than PAPP-A (i.e. it has higher sensitivity) 9,10.
Placental Growth Factor (PlGF) for Early Onset Pre-Eclampsia (EO-PE) Screening 13,14,15
PlGF is a glycoprotein that belongs to the vascular endothelial growth factor (VEGF) subfamily. It is a potent angiogenic factor. It is expressed in the villous syncytiotrophoblast and in the media of larger stem vessels in the human placenta. PIGF, together with VEGF, regulates the development of the placental vasculature, and the result depends on intra-placental oxygen pressure 13,14,15.
PlGF concentrations increase throughout pregnancy, peaking during the third trimester, and falling thereafter, probably as a consequence of placental maturation. In PE or intrauterine growth restriction (IUGR), changes in expression or function of PIGF, as well as some other angiogenic factors, may interrupt the function of the utero-placental unit, and thus contribute to many adverse obstetric outcomes 13,14,15.
Why PlGF?
Several studies have shown that women who subsequently develop PE have significantly lower maternal PlGF concentrations in the first trimester than those with normal pregnancies 22,23.
A systematic review and meta- analysis demonstrated that PlGF is superior to the other biomarkers for predicting PE 24. Serum PlGF biomarker can identify up 75% of women who develop pre-term PE with delivery at <37 weeks’ gestation and 90% of those with early PE at <32 weeks, at a screen-positive rate of 10%.
The COMPARE 16 Study
states that the high negative predictive values (NPV) support the role of PlGF-based tests as ‘rule-out’ tests for PE. Among the tests compared, the DELFIA Xpress® PlGF 1-2-3™ assay has the highest NPV.
ASPRE Study 17:
Using PlGF 1-2-3™ assay (PerkinElmer) in PE screening, ASPRE was the biggest prospective, randomised, placebo controlled trial that showed that use of aspirin was associated with a significant 62% reduction in the incidence of pre-term PE (<37 weeks GA) and an 82% reduction in the incidence of EO-PE (<34 weeks GA).
Recently, studies 15,18,19,20 showed that the administration of aspirin in pregnancies at high risk of PE reduces the length of stay in the neonatal intensive care unit (NICU) by about 70% mainly through the prevention of EO-PE.
When to offer?
The optimal time for screening is 11-13+6 weeks of gestation.
Who to offer?
Patients with high blood pressure, advanced age pregnancy, high BMI, positive history of pre-eclampsia or eclampsia, diabetes or kidney disease, multiple pregnancies or IVF assisted pregnancies.
The PlGF test can be offered to pregnant women of any age or risk category. It can be ordered for all naturally conceived or in vitro fertilisation (IVF) singleton or twin pregnancies, including those with egg donors. PlGF test is currently viewed as a screening test and clinical interpretation is always recommended 13,14.
Can it be offered with cFTS?
Yes, the same blood sample can be used for the measurement of biochemical markers for both pre-eclampsia screening and aneuploidy Down syndrome screening.
Specimen Requirements:
Plain tube or serum gel 7 ml
• The Placental Growth Factor (PlGF) costs $50
• Blood samples can be collected at any of our Australian Clinical Labs pathology collection centres
For assistance please call Biochem Dep. on (03) 9538 6790 or FTS (MSS) service on 0429116049
References
1. Tranquilli AL et al. The classification, diagnosis and management of the hypertensive disorders of pregnancy: A revised statement from the ISSHP. Pregnancy Hypertens 2014;4:97-104.
2. Wright D et al. A competing risks model in early screening for preeclampsia. Fetal Diagn Ther. 2012;32(3):171-178.
3. Wright D et al. Competing risks model in screening for preeclampsia by maternal characteristics and medical history. Am J Obstet Gynecol 2015;213:62.e1-10.
4. Poon et al. The International Federation of Gynecology and Obstetricians (FIGO) Initiative on Pre-Eclampsia: A pragmatic Guide for First Trimester Screening and Prevention. Int J Gynecol Obstet 2019;145 (Suppl. 1): 1–33.
5. Parker S et.al. Updated National Birth Prevalence estimates for selected birth defects in the United States, 2004-2006. Birth Defects Res A Clin Mol Teratol. 2010.
6. WHO media centre, fact sheet 2016. http://www.who.int/mediacentre/factsheets/ fs363/en/
7. Duley L. The global impact of pre-eclampsia and eclampsia. Semin Perinatol. 2009.
8. Romo A et al. Intrauterine growth retardation (IUGR): epidemiology and etiology. Pediatr Endocrinol Rev. 2009.
9. Tsiakkas A et al. Serum placental growth factor in the three trimesters of pregnancy: effects of maternal characteristics and medical history. Ultrasound Obstet Gynecol 2015;45:591-598.
10. Wright A et al. Maternal serum PAPP-A and free β-hCG at 12, 22 and 32 weeks’ gestation in screening for pre-eclampsia. Ultrasound Obstet Gynecol 2016;47:762-767.
11. Poon LC et al. Protocol for measurement of mean arterial pressure at 11-13 weeks’gestation. Fetal Diagn Ther 2012;31:42-48.
12. O’Gorman N et al. Uterine artery pulsatility index at 12, 22, 32 and 36 weeks’ gestation in screening for pre-eclampsia. Ultrasound Obstet Gynecol 2016;47:565-567.
13. Royal College of Obstetricians and Gynaecologists patient information leaflet, Information for you: Pre-eclampsia. RCOG Patient Information Committee, London, UK, Aug 2012.
14. Rolnik DL et al. Nicolaides KH. ASPRE trial: performance of screening for preterm pre-eclampsia. Ultrasound Obstet Gynecol Jul 25, 2017.
15. Bujold E et al. Prevention of preeclampsia and intrauterine growth restriction with aspirin started in early pregnancy: a meta-analysis. Obstet Gynecol. 2010;116:402-414.
16. McCarthy FP et al. Comparison of three commercially available placental growth factor tests in women with suspected preterm pre-eclampsia: the COMPARE study. Ultrasound Obstet Gynecol 2019;53:62-67.
17. Rolnik DL et al. ASPRE trial; Aspirin versus Placebo in Pregnancies at High Risk for Preterm Preeclampsia.N Engl J Med. 2017 Aug 17;377(7):613-622.
18. Roberge S et al. Early administration of low-dose aspirin for the prevention of preterm and term preeclampsia: a systematic review and meta-analysis. Fetal Diagn Ther.2012;31(3):141-146. doi:10.1159/000336662. Epub 2012 Mar 21.
19. Roberge S et al. The role of aspirin dose on the prevention of preeclampsia and fetal growth restriction: systematic review and meta-analysis. Am J Obstet Gynecol. 2017 Feb;216(2):110-120.e6.
20. Wright D et al. Secondary analysis of ASPRE trial. Am J Obstet Gynecol. 2018;612.e6.
21. PerkinElmer PlGF assay product inserts 13908271, 13907817.
22. Chau K et al. Placental growth factor and pre-eclampsia. J Hum Hypertens. 2017;31:782–786.
23. Wortelboer EJ et al. Longitudinal trends in feto-placental biochemical markers, uterine artery pulsatility index and maternal blood pressure during the first trimester of pregnancy. Ultrasound Obstet Gynecol. 2011;38:383–388.
24. Zhong Y et al. Serum screening in first trimester to predict preeclampsia, small for gestational age and preterm delivery: Systematic review and meta-analysis. BMC Pregnancy Childbirth. 2015;15:191.
25. https://www.ranzcog.edu.au/Womens-Health/Patient-Information-Resources/Pre-eclampsia-and-High-Blood-Pressure-During-Pregn
26. NHMRC National Health and Medical Research Council, October 2017. Evidence Based Recommendations
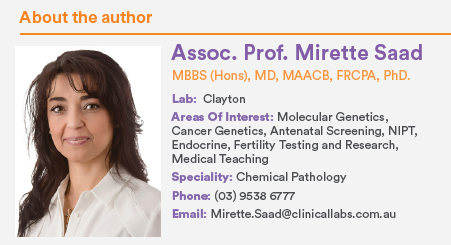
Associate Professor Mirette Saad is a Consultant Chemical Pathologist and the National Clinical Director of Molecular Genetic Pathology at Australian Clinical Labs. Associate Professor Mirette Saad’s PhD research allowed her to gain unique experience in a wide range of biochemical, molecular genetics and cancer targeting. At Clinical Labs, Associate Professor Saad leads the antenatal screening program including combined First Trimester Screening and Non-Invasive Prenatal Testing (NIPT) along with the Molecular Genetic testing for hereditary disorders, personalised drug therapy somatic mutation and gene expression profile testing in cancer.



