Patients’ vitamin D levels drop significantly during winter.
By Dr David Deam
Published September 2019
Vitamin D levels fluctuate significantly depending on the season, especially in the Southern states of Australia. At the end of winter, approximately 36% of Australians are vitamin D deficient, in comparison to 14% at the end of summer. Therefore, making the end of winter the best time to test patients for vitamin D deficiency.
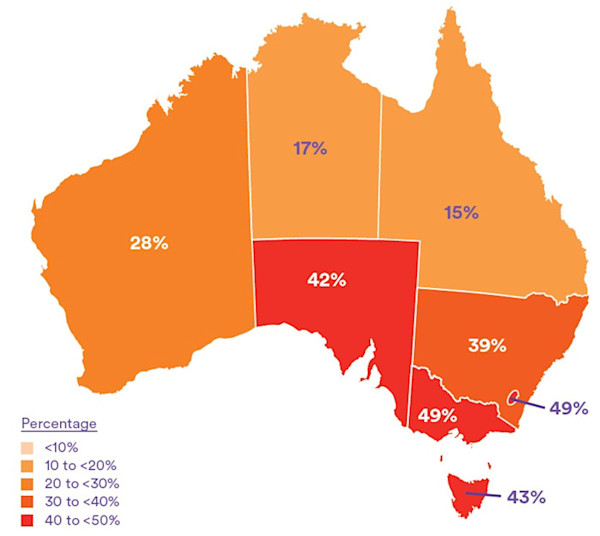
The below diagrams indicate the percentage of Australians with a vitamin D deficiency in summer (diagram 1) versus winter (diagram 2).
Diagram 1 - Vitamin D deficiency in summer by state (2011-2012)
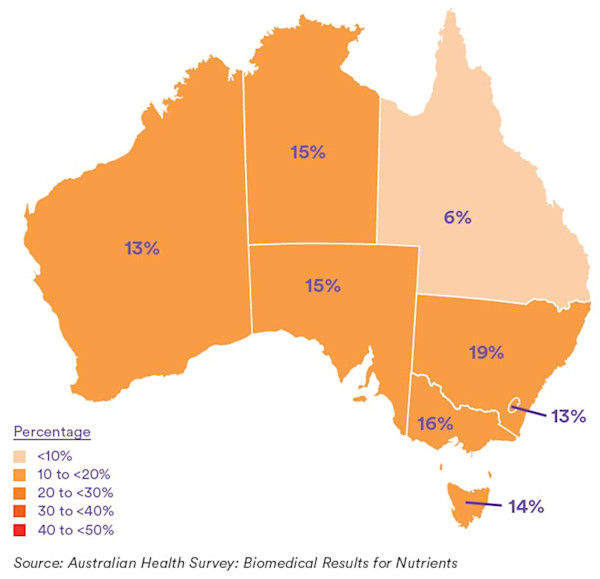
Diagram 2 - Vitamin D deficiency in winter by state (2011-2012)
Health implications of vitamin D deficiency
Vitamin D deficiency is of concern as it can lead to a variety of health conditions including the loss of bone density, which can contribute to osteoporosis and fractures in adults and rickets in infants and children. Low levels of vitamin D have also been found in association with other health conditions, such as cardiovascular disease, diabetes, immune system diseases, microbial and respiratory diseases, cognitive impairment in older adults, mental health and cancer.
Target vitamin D levels
The international recommendations for adequate vitamin D levels vary, but based on a review of current literature and recently published recommendations 1, 2 Clinical Labs suggests that adequate vitamin D status is a serum level equal to, or greater than, 50 nmol/L at the end of winter. This level should be 10-20 nmol/L higher at the end of summer to allow for seasonal decrease.
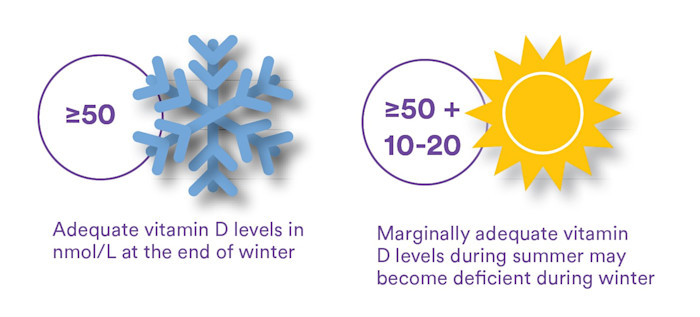
This figure is based on the level below which parathyroid hormone concentrations begin to rise and the risk of fractures increases.
As for all tests, Australian Clinical Labs’ pathologists and scientists will continue to evaluate current literature and our target range may change as new evidence emerges.
Who to test
Vitamin D testing should be ordered for patients at risk of vitamin D deficiency, including:
- Housebound people - including the sick and disabled
- Elderly in high care
- People with darker skin
- People who cover their skin due to religious or cultural reasons
- People who regularly avoid the sun
- People who work indoors
Also patients with:
- Signs, symptoms and/or planned treatment of osteoporosis or osteomalacia
- Increased alkaline phosphatase with otherwise normal LFTs
- Hyperparathyroidism, hypo- or hypercalcaemia or hypophosphataemia
- Malabsorption (i.e. CF, IBD, coeliac, etc)
- Medications known to decrease vitamin D levels (i.e. anticonvulsants)
- CRF and transplant recipients
Vitamin D testing
Vitamin D testing at Clinical Labs measures the concentration of total 25-hydroxyvitamin D (25-OHD) in a patient’s serum. The report will also include previous test results, for comparison (if applicable), and suggested cut points to define sufficient, deficient and severely deficient vitamin D levels.
Treatment
To ensure adequate levels of vitamin D are maintained throughout the year, the following sun exposure times (mins per day) are recommended for 1/3MED for moderate fair skin, at either 10am or 2pm daily.3
| December-January | July-August | |
|---|---|---|
| Perth | 5-6 mins | 20-28 mins |
| Adelaide | 5-7 mins | 25-38 mins |
| Melbourne | 6-8 mins | 32-52 mins |
| Hobart | 7-9 mins | 40-47 mins |
| Sydney | 6-8 mins | 26-28 mins |
| Brisbane | 6-7 mins | 5-19 mins |
| Cairns | 6-7 mins | 9-12 mins |
If patients are unable, for a variety of reasons, to gain the required amount of sun exposure for vitamin D production, supplementation may be required.
A maintenance dose of up to 1000 IU/day may be adequate, however some individuals will require higher doses. Severe vitamin D deficiency (serum level <20 nmol/L) may require 3000-5000 IU/day for 6-12 weeks.
Supplements should be vitamin D3. Adequate dietary calcium is also required, at least 1g/day and up to 1.3g/day, for older adults. Many patients will require supplementation to achieve this amount.
Note: Calcium supplements are best taken before sleep to ensure maximum absorption and suppression of peak bone turnover which usually occurs between approximately 2am and 3am.
If you enjoyed this article, subscribe to our electronic Pathology Focus newsletter.
How to Order Vitamin D Testing
Note the reason for testing to meet Medicare eligibility criteria for bulk-billing in the ‘Clinical Notes’ section on a Clinical Labs General Pathology Request Form.
Blood samples can be collected at any Clinical Labs collection centre.
Due to the long half-life, repeat testing should not be performed earlier than 3 months after either starting or changing the dose of vitamin D supplements.
Serum calcium, phosphate and parathyroid hormone will assist in placing the vitamin D level within the context of overall calcium homeostasis.
If osteoporosis is present, assessment of bone turnover markers (fasting C-terminal telopeptide of type 1 collagen [CTX] and procollagen type 1 N propeptide [P1NP]) may be considered to provide a way of monitoring bone turnover in response to therapy.