By Dr Joel Pinczewski
The clinical information and biopsy type that clinicians provide to pathologists can be critical in ensuring a correct diagnosis in skin biopsies. This is true for both neoplastic and inflammatory skin lesions. In previous articles my colleagues have provided some biopsy recommendations for different types of skin lesions. In this article, I will discuss diagnostic pitfalls that can occur when inadequate biopsies are provided as well as the importance of clinicopathologic correlation when interpreting skin biopsies.
Basal cell carcinoma
I will begin by discussing basal cell carcinoma (BCC). Basal cell carcinoma is the most common type of skin malignancy. It includes more aggressive and less aggressive subtypes, as shown in Table 1. Diagnosing a basal cell carcinoma is generally quite straightforward. However, there are histologic mimics of basal cell carcinoma and misdiagnoses can occur, particularly in the setting of small biopsies containing ulcerated skin or in very superficial biopsies.
For example, dermatofibromas can contain areas of basal cell hyperplasia (a type of benign reactive process). Basal cell hyperplasia typically does not pose a diagnostic dilemma for experienced dermatopathologists. However, less experienced pathologists do sometime mistake it for a basal cell carcinoma, particularly in very superficial biopsies. Collision tumours – a mixture of basal cell carcinoma and dermatofibroma – can also occur, so not all basaloid lesions occurring in dermatofibromas are benign. The RACGP website includes a case report of such a collision tumour1.
Among the malignant lesions that can be mistaken for basal cell carcinoma, melanoma and merkel cell carcinoma are two examples. The prognosis and clinical management of both melanoma and merkel cell carcinoma are significantly different from basal cell carcinoma. Therefore, a misdiagnosis of either would have potentially profound clinical consequences for a patient.
Another issue with superficial biopsies is that they make it difficult to identify subtypes of basal cell carcinoma. This is because superficial biopsies often prevent assessment of architectural features in basal cell carcinomas. Therefore, for example, an infiltrative growth pattern may not be evident in a superficial biopsy. I often see examples of infiltrative basal cell carcinoma in excision specimens which were incorrectly classified as nodular type basal cell carcinoma in the original superficial shave biopsy of the lesion.
Table 1. BCC subypes
| Less aggressive subtypes | More aggressive subtypes |
|
|
The type of biopsy that a clinician provides can also be significant in diagnosing superficial and multifocal type basal cell carcinomas since this type of basal cell carcinoma has skip areas between nests of malignant cells, as shown in Figure 1. This means that a narrow punch biopsy may not contain malignant cells, particularly if the reporting pathologist has not examined multiple levels of tissue. The gaps between nests of malignant cells in superficial and multifocal basal cell carcinomas also makes it difficult to confirm margin status in narrowly excised lesions.
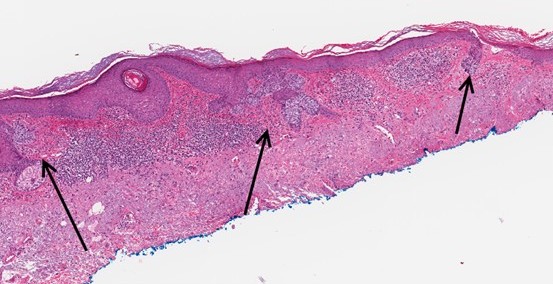
Figure 1. Superficial and multifocal basal cell carcinoma.
Squamous cell carcinoma
Another common type of skin cancer is squamous cell carcinoma (SCC). Well differentiated squamous cell carcinoma can be a difficult diagnostic area since various mimics can occur. Specifically, reactive atypia can occur in response to trauma, infections and inflammation and this can be extremely difficult to differentiate from a well differentiated squamous cell carcinoma in narrow punch biopsies or in superficial biopsies. An examination of the medical literature reveals various papers describing the
difficulties in differentiating inflammatory lesions such as hypertrophic lichen planus from squamous cell carcinoma2. As a result, in inadequate biopsies, pathologists often use terminology such as “squamoproliferative lesion; well differentiated squamous cell carcinoma cannot be excluded” or “atypical squamous proliferation” when they cannot confidently confirm or exclude a diagnosis of squamous cell carcinoma. In order to minimise these types of non-committal diagnoses, it is best to provide the pathologists with an adequately sized biopsy and to also provide adequate clinical information.
Melanocytic lesions
Melanocytic lesions are another area where the nature of the biopsy is critical for an accurate diagnosis. I recently received two separate cases where an atypical melanocytic lesion had been curetted by clinicians. Unfortunately one of these was a large invasive malignant melanoma. Curette biopsies of melanocytic lesions create diagnostic difficulties for the pathologist and prevent assessment of margins. Fortunately, most clinicians understand that curettage of atypical melanocytic lesions is to be avoided.
Some clinicians choose to do small punch biopsies of atypical melanocytic lesions and this can also cause diagnostic difficulties. Melanomas can arise in naevi and these may be missed due to sampling issues in punch biopsies. Also, punch biopsies often prevent assessment of symmetry and circumscription, two important factors used in differentiating benign from malignant melanocytic lesions. The preferred biopsy technique for atypical melanocytic lesions is a narrow shave excision.
Ulcerated skin
Another issue that occurs quite commonly is clinicians sending biopsies of ulcerated skin to evaluate for suspected inflammatory or neoplastic skin lesions. Ulceration can pose difficulties in evaluating for both types of lesions. Sending a small/partial biopsy of ulcerated skin can cause diagnostic difficulties in squamoproliferative lesions. For example, if the clinical impression is squamous cell carcinoma in situ (Bowen’s Disease) then sending a biopsy of wholly ulcerated skin is not going to provide any useful diagnostic information. Ulceration can also pose diagnostic challenges in deeper lesions. This is because reactive atypia and epidermal hyperplasia can occur in the setting of ulceration, see Figures 2 & 3, and differentiating this from a well differentiated squamous cell carcinoma in a small/partial biopsy may be very difficult.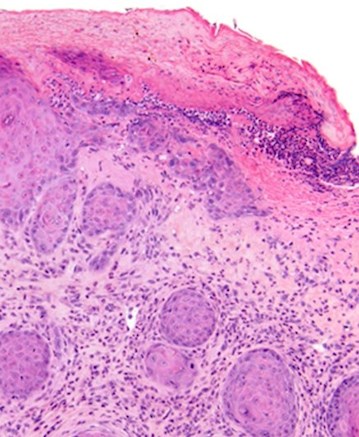
Figure 2. Is this lesion benign (reactive squamous hyperplasia) or it it a well differentiated squamous cell carcinoma?

Figure 3. A deeper biopsy revels that this lesion contains reactive squamous proliferation.
In regard to suspected inflammatory lesions, ulceration also causes diagnostic difficulty since reactive spongiosis and reactive inflammation typically occur in the vicinity of ulcerated skin. Clearly, there are some instances where taking a biopsy of ulcerated skin cannot be avoided, such as ulcerated solitary lesions. However, where possible, it is best not to biopsy ulcerated skin and especially not to send a biopsy containing only ulcerated skin without some intact epidermis.
Multiple biopsies
A couple of additional points that I would like to make are in terms of numbers of biopsies and types of biopsies. If an inflammatory lesion, an infection or a cutaneous lymphoma is suspected, then sending at least two biopsies is more likely to yield diagnostically useful findings and therefore an accurate diagnosis. This is because the findings in any one biopsy may not be representative due to sampling issues. For example, an insect bite reaction or some other incidental lesion may be sampled
inadvertently. If an immunobullous disease, such as bullous pemphigoid is suspected or for suspected vasculitis, it is best to also include a biopsy of fresh peri-lesional tissue in saline soaked gauze or Michel’s transport medium so that immunofluorescence staining can be performed.
The importance of providing adequate clinical information
Clinicopathologic correlation is also very important in many instances. Certainly in the setting of inflammatory lesions it is important to provide the pathologist with suitable and accurate clinical information. Please be careful when using terms like “rash”. Some clinicians use this term very loosely. For example, it is not uncommon to receive a biopsy of a basal cell carcinoma with the clinical history of “rash”. Please specify in the clinical information whether you suspect a lesion to be neoplastic or inflammatory in nature. Please also indicate whether the lesion you are sampling is solitary or whether the patient has multiple similar lesions. Other important information includes: the colour, size, shape, onset and duration of the lesion. For inflammatory lesions please indicate if there is any known association. For example, has the patient started a new medication. Please indicate if the lesion is painful or itchy. Clinical photographs can also be very helpful in some cases.
Adequate clinical information is also important when evaluating neoplastic skin lesions and in particular for melanocytic lesions. For example, if there is a known history of trauma please include this in the clinical information. Traumatisation can potentially explain atypical finding in a melanocytic lesion. This is because reactive atypia is a common feature of recurrent naevi. The atypia in recurrent naevi can closely mimic a malignant melanoma, particularly in a partially sampled melanocytic lesion. Diagnosing recurrent naevi can be difficult without adequate history in partially biopsied melanocytic lesions.
References
1. Mortimer and Muir. Basal cell carcinoma in dermatofibroma dual diagnosis AJGP Vol. 49, No. 12, 2020.
2. Shao, Carew and Muir. Hypertrophic lichen planus mistaken for squamous cell carcinoma. Med J Aust 2018; 209 (10).
About the author:

Dr Joel Pinczewski
MD (USA) PhD FRCPA
Lab: Clayton
Speciality: Anatomical Pathology
Areas of Interest: Melanocytic lesions, adnexal tumours and inflammatory lesions
Phone: 1300 134 111
Email: joel.pinczewski@clinicallabs.com.au
Dr Joel Pinczewski obtained a PhD in virology from Monash University. Soon after he moved to the United States where he completed his postdoctoral training at the National Institutes of Health. Dr Pinczewski subsequently completed medical school at the Saba University School of Medicine and a residency in Anatomical and Clinical Pathology at the University of Maryland. He then completed a dermatopathology fellowship at the University of Virginia where he trained with two of the leading dermatopathologists in the United States. Dr Pinczewski is certified in Anatomic, Clinical and Dermatopathology by the American Board of Pathology. He is also a fellow of the Royal College of Pathologists of Australasia (FRCPA). Dr Pinczewski has published numerous articles in the medical literature. He is a passionate teacher and researcher and has delivered lectures in dermatopathology both nationally and internationally. Dr Pinczewski is skilled in all areas of dermatopathology.
Local pathologists near you:

Dr Asokan Pasupathy
MBBS D. Path MD FRCPA
Lab: Bella Vista
Speciality: Anatomical Pathology
Areas of Interest: Breast, skin, GIT and uropathology
Phone: (02) 8887 9919
Email: asokan.pasupathy@clincallabs.com.au
Dr Asokan Pasupathy graduated from the University of Jaffna, Sri Lanka in 1994. He completed his postgraduate pathology training through the Postgraduate Institute of Medicine, University of Colombo, Sri Lanka in 2004. After moving to Australia, Dr Pasupathy completed further training in anatomical pathology at Liverpool and Westmead Hospitals in Sydney. Asokan obtained his fellowship in 2010 and joined NSW Health Pathology, Nepean Hospital and then Tamworth Hospital. Dr Pasupathy recently joined Clinical Labs working at our Bella Vista laboratory in NSW. Although his special interests in pathology include breast pathology, dermatopathology, GIT pathology and uropathology, Asokan generally reports all areas of anatomical pathology and cytopathology cases.
Dr Aaron Andreas
MBChB(Hons) Genetics BS(Hons) FRCPath
Lab: Subiaco
Speciality: Anatomical Pathology
Areas of Interest: Gastrointestinal, pancreatic, skin, soft tissue and sarcoma pathology
Phone: (08) 9213 2173
Email: aaron.andreas@clinicallabs.com.au
Dr Aaron Andreas graduated from the University of Liverpool in 2014 with MBChB (Honours) and Genetics BSc (Honours) degrees. Aaron began his training in pathology at Leeds Teaching Hospitals in the United Kingdom, achieving fellowship of the Royal College of Pathologists (UK) in 2021. Aaron subsequently gained post-fellowship experience at Leeds Teaching Hospitals in gastrointestinal, pancreatic, skin, soft tissue and sarcoma pathology. Aaron has most recently been working as a Consultant Histopathologist at Bradford Teaching Hospitals in Yorkshire specialising in skin, upper and lower gastrointestinal pathology and non-gynaecological cytopathology. Aaron also has experience of digital pathology reporting. Aaron is passionate about pathology and enjoys teaching related to pathology. He has contributed to undergraduate teaching at the University of Leeds School of Medicine for several years as a visiting tutor and, more recently, to postgraduate teaching as a visiting lecturer on the FRCR oncology course lecturing on gastrointestinal malignancy. Aaron also enjoys public engagement related to pathology and has volunteered as an anatomy demonstrator to deliver dissection sessions to primary and secondary school age children.