By Associate Professor Chris Barnes
Most people infected with COVID-19 will fully recover within a few weeks of infection. In a study of almost 3,000 patients with COVID-19 infection from NSW, 80% of patients had fully recovered by 30 days. However, up to 5% of patients will continue to have symptoms beyond 12 weeks following infection.1
There is no agreed definition of “Long COVID” syndrome. The WHO (World Health Organization) has provided a clinical case definition for “post COVID-19 condition”. This definition includes patients with a range of potentially overlapping and intermittent symptoms including fatigue, shortness of breath, and cognitive dysfunction, that impact everyday functioning. The symptoms extend beyond 12 weeks from COVID-19 infection and are present for at least 2 months.2 There is limited understanding of the pathogenesis and risk factors for patients developing Long COVID.
There is an absence of well-established evidence-based guidelines for the investigation and management of patients presenting with potential Long COVID. Clinicians may be faced with the diagnostic and management dilemma of how best to approach patients suspected of having Long COVID syndrome. Tertiary referral centres are being inundated with patients suspected of having Long COVID syndrome, with some patients being forced to wait up to one year before being seen.3
Clinical assessment of patients presenting with symptoms suggestive of Long COVID syndrome can be difficult. Symptoms can be varied and overlapping, often without objective clinical signs. The NICE (The National Institute for Health and Care Excellence) guideline on Long COVID includes commonly reported symptoms, which can be classified as follows.4
Commonly reported “Long COVID” symptoms
|
Respiratory / ENT and Cardiovascular symptoms |
|
|
|
|
Generalised and Neurological symptoms |
|
|
|
|
Gastrointestinal symptoms |
|
|
|
|
Musculoskeletal / skin symptoms |
|
|
|
In the setting of high clinical demands, self-report questionnaires have been proposed as a potential guide to support clinical decision-making. The Symptom Burden Questionnaire™ for Long COVID (SBQ™-LC) is a comprehensive patient-reported outcome tool measuring the frequency and severity of symptoms in patients with Long COVID.5 This questionnaire highlights the varied range of symptoms of patients presenting with Long COVID and includes 17 independent scales with a summed raw score, which can be transformed to a linear (0-100) score with higher scores associated with higher disease burden.
Recommended laboratory investigations
Download Long COVID Brochure
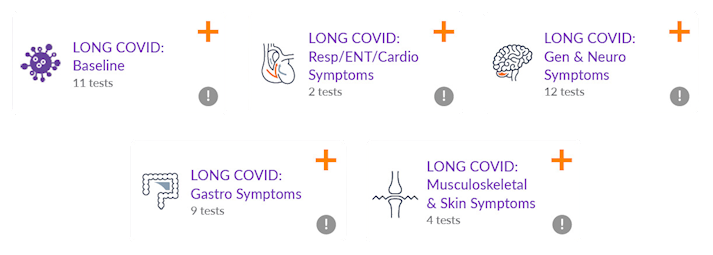
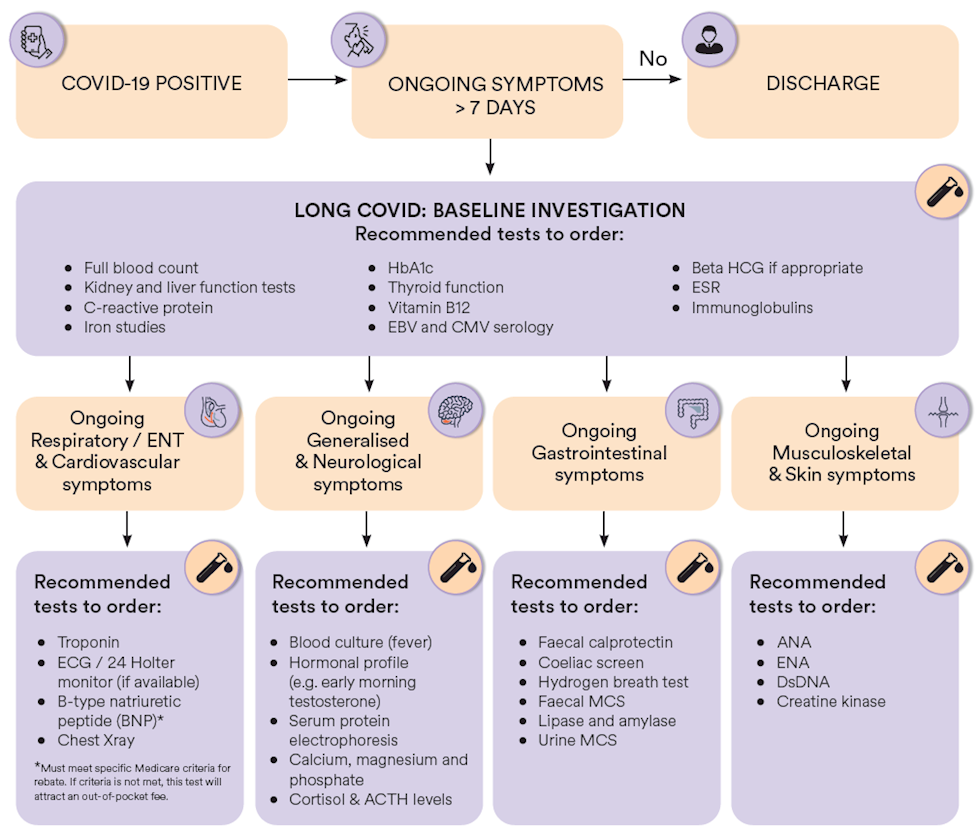
Targeted laboratory investigations are essential in supporting the assessment of patients presenting with symptoms suggestive of Long COVID. It is important to acknowledge that the variety of potential symptoms of patients presenting with Long COVID may make excluding underlying medical conditions difficult. Additionally, comorbidities that require targeted therapy may compound symptoms of Long COVID. The approach below is suggested to support the investigation of patients presenting with potential Long COVID with an initial baseline series of investigations followed by a more targeted methodology directed towards the patients’ symptoms.
|
Baseline investigations |
||
|
|
|
PATIENTS PRESENTING WITH:
|
Respiratory / ENT |
Generalised and |
Gastrointestinal |
Musculoskeletal / |
|
|
|
|
Summary of Long COVID investigative recommendations
References
1. Liu B, Jayasundara D, Pye V, Dobbins T, Dore GJ, Matthews G, et al. Whole of population-based cohort study of recovery time from COVID-19 in New South Wales Australia. (2666-6065 (Electronic)).
2. WHO. A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021 2021 [Available from: https://www.who.int/publications/i/item/WHO-2019-nCoVPost_COVID-19_condition-Clinical_case_definition-2021.1.
3. Mannix L. Long COVID clinics ‘inundated’ with patients, and doctors can’t cope. Sydney Morning Herald. 2022.
4. Shah W, Hillman T, Playford ED, Hishmeh L. Managing the long term effects of covid-19: summary of NICE, SIGN, and RCGP rapid guideline. BMJ. 2021;372:n136.
5. Hughes SE, Haroon S, Subramanian A, McMullan C, Aiyegbusi OL, Turner GM, et al. Development and validation of the symptom burden questionnaire for long covid (SBQLC): Rasch analysis. BMJ. 2022;377:e070230.
Covid-19 and Urinary Symptoms
The COVID-19 pandemic has raised concerns about its potential impact on various body systems, including the urinary tract. Recent studies suggest that elderly patients with COVID-19 may experience urinary symptoms, such as urinary incontinence, urgency, frequency, and hematuria. This could be due to the direct or indirect effects of COVID-19 on the urinary tract or as a result of the systemic inflammatory response triggered by the virus.
It is important to note that urinary symptoms alone are not specific to COVID-19 and could be caused by other medical conditions, such as urinary tract infections, prostate enlargement, or bladder dysfunction. However, given the potential overlap of symptoms and the severity of the COVID-19 pandemic, it may be helpful to test for COVID-19 when elderly patients present with urinary symptoms.
Timely diagnosis of COVID-19 in these patients may facilitate appropriate management and prevent the spread of the virus to other vulnerable individuals. Healthcare providers should remain vigilant and consider COVID-19 testing in elderly patients with urinary symptoms, particularly if they have been exposed to the virus or have other risk factors for COVID-19. It is also essential to provide comprehensive care and support to older adults with COVID-19 and urinary symptoms to prevent further complications and improve their overall health outcomes.
References
1. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7995211/
2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9233460/
3. https://www.nature.com/articles/s41585-022-00586-1
Single-click ordering for “Long COVID” Test Profiles available with Clinical Labs eOrdersFor clinics using Best Practice, MedicalDirector Clinical or Clinical Labs eResults. Instead of adding each test individually, click through to our eOrders screen and navigate to ‘Clinical Recommendations’ (MD) or ‘Clinical details’ (BP), where you will find the Long COVID test profiles described above pre-configured, and can be ordered with the click of a button. Test profiles can also be searched for via the main eOrders search bar. |
About the author:
 Assoc. Prof. Chris Barnes
Assoc. Prof. Chris Barnes
MBBS FRACP FRCPA
Lab: Clayton
Speciality: Haematology
Areas of Interest: Paediatric haematology, nonmalignant haematological conditions including thrombosis and bleeding disorders
Phone: (03) 9538 6777
Email: chris.barnes@clinicallabs.com.au
Associate Professor Chris Barnes is the National Director of Haematology and provides strategic direction for haematology at Clinical Labs on a national level. He is a clinical and laboratory-trained haematologist who has been part of Melbourne Haematology and has worked with Clinical Labs (and previously Healthscope) for several years. A/Prof Barnes is also the director of the Haemophilia Treatment Centre at the Royal Children’s Hospital, and has experience in management and leadership positions. He has an active clinical research interest and serves as the director of both Melbourne Haematology (Clinical) and Melbourne Paediatric Specialists.