Cardiac Testing and Arrhythmias in General Practice
Written by Dr Christopher Goods.
Dr Christopher Goods is an interventional cardiologist with a special interest in ischemic heart disease. Here, he discusses the effectiveness of Holter monitors for patients presenting with heart irregularities, as well as the important role that GPs play in this area of analysis and care. Holter monitors are universally regarded as the first-line test for assessing cardiac issues: they are a small, batter-powered device worn by the patient for 12-48 hours as they go about their daily lives. Much like an ECG, the device uses electrodes and leads to pick up a patient’s heart-rate and heart rhythm, as well as record when they experience chest pains or arrhythmias. An inexpensive, painless and non-invasive test, there is good reason as to why clinical use of the device is widespread – and, fortunately, the vast majority of GPs are well across Holter monitors’ efficacy and value.
When to use a Holter monitor

Holter monitors are the undisputed, the simplest and the best investigation tool we have to look for intermittent arrhythmias. We also use it for people that are experiencing exertion-related shortness of breath, dizziness and chest pains – because sometimes those symptoms can be a result of underlying heart problems that patients cannot necessarily feel in the first instance. If a patient is short of breath, it can be due to arrhythmias, both fast or slow heartbeats, or tachyarrhythmia.
We also tend to see a lot of young people presenting to our practice with anxiety issues or heartbeat irregularity which we often find is due to alcohol or caffeine consumption. These individuals are prime candidates for Holter monitoring – healthy, young people who we don’t usually expect to have underlying, organic disease. Instead, in most cases, our monitoring just finds some ectopic beats or tachycardia or periods of increased heart rate.
As noted above, Holter monitors are most commonly used for patients over the course of a day or two. However, if a patient is experiencing quite infrequent arrhythmias, we sometimes choose to undertake a longer period of analysis – for example, a seven-day event monitor. In extreme cases, we may even refer the patient on for an electrophysiology study, where an electrical cardiologist (or electrophysiologist) uses electrical intervention to stimulate the heart and bring on the arrythmia. But this is quite rare, and regular use of Holter monitors is definitely the most effective tool as far as it goes for arrhythmias.
From a patient’s point of view

When we first propose Holter monitoring to patients, and explain that the machines must be worn at all times during the assessment period (including during sleep), the immediate misconception is that they will need to stay in a laboratory overnight. But like anything, education is key. We begin by explaining that Holter monitoring is painless and non-invasive and that, while wearing the device, they can go about most of their routine, daily activities. There are a few limitations they should be made aware of, for instance, patients can shower but they cannot go swimming, and we prefer they don’t use moisturising cream as the electrodes won’t stick.
Clinicians will often ask that patients keep a diary of all their activities while wearing the monitor, including the start time and duration for each. Similarly, any specific symptoms they experience when wearing the monitor should be recorded as well. The more information for the clinician assessing their Holter results, the better.
Interpreting the data and next steps
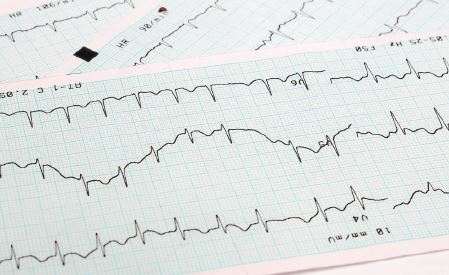
Once the monitoring period concludes, Holter devices allow clinicians to send the data off for analysis to determine any variations or inconsistencies. As you can imagine, the device creates a significant amount of data, so it is very much computer-assisted. So while a technician or clinician does have the option of going through an entire report (eg., the full 24- or 48-hour period), the analysis program will zero in on any specific inconsistencies and irregularities.
Most of the time, the results of Holter monitoring will show no major, underlying cardiac conditions. I would say that about 95 per cent of the time, we are able to assure the patient that everything looks quite normal. However, there are obviously instances where the data reveals an issue that requires treatment. This will usually come in the form of medication, however, in severe cases, a patient may require a pacemaker.
I often say that there is an art in determining which patients require a pacemaker to be installed, as there can
be grey areas when assessing Holter results. The worst outcome would be if you recommend a pacemaker be installed and then the patient continues to experience fainting due to another issue or health complication. As a result, correct interpretation of Holter data is crucial.
The role of GPs in cardiac testing
Generally, cardiologists prefer that patients presenting with the common warning signs discussed above – palpitations, irregular heartbeats, shortness of breath, and so on – actually undertake Holter testing from their GP before they are referred on. In this case, the patient can get a Holter, undertake the assessment period, and then as they wait to see a cardiologist, the cardiologist already has the data and results on-hand. This would take away a step in the diagnostic process, allowing the cardiologist to make the most informed judgement from the outset.
About the Author