By Associate Professor Chris Barnes
Iron deficiency is the most common cause for anaemia across all populations and is estimated to affect up to 2 billion worldwide1. Patients presenting with iron deficiency is a common diagnostic and management problem, and iron deficiency in females is particularly common due to the increased iron requirements associated with menstruation and pregnancy.
Symptoms of iron deficiency
Iron is essential to several biological functions, including energy production via mitochondrial metabolism, enzymatic processes involving neurotransmitters, and skeletal and cardiac muscle, and immune-based processes. This is in addition to haemoglobin mediated delivery of oxygen. This explains the common and varied symptoms associated with iron deficiency including lethargy, fatigue, brain fog (occasionally described misogynistically as “mummy brain”), restless legs, pica, and hair loss. These symptoms of iron deficiency occur prior to the development of iron deficiency anaemia, because iron stores are depleted initially from the liver and then from other iron enzymes and proteins in order to preserve erythropoiesis.
Iron deficiency anaemia will develop gradually over time, and patients may present with marked anaemia as low as 30 g/L. Whilst physiological compensation may occur, patients with marked iron deficiency anaemia may be at risk of cardiovascular instability including heart failure.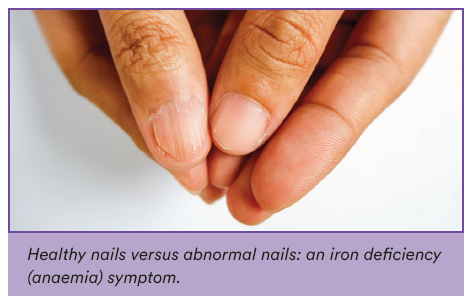
The impact of menorrhagia on iron levels
The most common risk factor associated with iron deficiency in females is menorrhagia. Whilst the average age at menarche is 13.8 years, menarche as early as 9 years may be considered normal and is influenced by both genetic and nutritional factors. The volume of menstrual blood loss may be difficult to accurately assess. Functional measures including asking about the passing of large clots, the need for double menstrual products to avoid flooding, the need to change products overnight, or concern about flooding during the day can all be used to assess for the presence of menorrhagia2.
Benefits of iron studies in diagnosing iron deficiency
Laboratory tests to screen for iron deficiency in female patients can be helpful as a part of good clinical practice even in the absence of symptoms of menorrhagia. Anaemia secondary to iron deficiency can be identified in up to 18% of otherwise healthy women, whereas iron deficiency (in the absence of anaemia) was present in 48% of 271 “asymptomatic” women participating in a
community running event3.
A complete assessment of iron studies is recommended as an important first step in the investigation of patients with potential iron deficiency. Whilst an isolated low serum ferritin test is an adequate test if the patient is otherwise well, it is well known that ferritin is an acute phase reactant and may be falsely elevated in acute and chronic inflammation, fatty liver, raised BMI, or in the setting of OCP use. Additional laboratory markers available when ordering iron studies may be helpful in the assessment
of iron deficiency; a low transferrin saturation (<20%)supports a diagnosis of iron deficiency in patients with concomitant inflammation or systemic illnesses (even in the presence of a normal serum ferritin).
Below is a table to assist in the interpretation of iron studies in females presenting with risk factors or symptoms suggestive of iron deficiency.
| Iron | Transferrin saturation |
Ferritin | Soluble transferrin receptor |
|
| Iron deficiency | Decreased | Decreased | Decreased | Increased |
| Iron deficiency + acute phase response |
Decreased | Normal or decreased |
“Normal” <100μg/L |
Increased |
| Acute phase response |
Decreased | Decreased | Increased | Normal |
| Iron overload | Increased | Increased | Increased | Decreased |
Clinical Labs iron studies reference ranges
The table below details the reference ranges for Clinical Labs iron studies testing for female patients.
| TEST | GENDER | AGE | LOWER LIMIT | UPPER LIMIT |
| IRON SERUM | F & M | All | 10 | 30 |
| TRANSFERRIN | F & M | All | 2.1 | 3.8 |
| IRON SATURATION | F | All | 15 | 45 |
| FERRITIN SERUM | F & M | 6m - 15 years | 20 | 140 |
| FERRITIN SERUM | F | 15 - 50 years | 30 | 200 |
| FERRITIN SERUM | F | >50 years | 30 | 300 |
Treatment
Treatment of iron deficiency should focus on the underlying cause including consideration of any sources of bleeding
including menorrhagia, polymenorrhoea, or occult gastrointestinal blood loss. Iron supplementation in either oral or parenteral form is required after sources of blood loss have been addressed.
Oral iron supplementation may be associated with a high risk of gastrointestinal symptoms including nausea and abdominal pain. Second daily oral iron supplementation may reduce the incidence of the effects and may be associated with improvement in hepcidin-mediated iron absorption4.
Parenteral iron therapy has the potential to rapidly increase iron stores and with the availability of parenteral preparations that are associated with less risk of acute reactions, are an acceptable and attractive alternative to consider in females presenting with iron deficiency5.
References
1. Camaschella C. Iron-Deficiency Anemia. N Engl J Med. 2015;373(5):485-6.
2. Fraser IS, Mansour D, Breymann C, Hoffman C, Mezzacasa A, Petraglia F. Prevalence of heavy menstrual bleeding and experiences of affected women in a European patient survey. Int J Gynaecol Obstet. 2015;128(3):196-200.
3. Dugan C, MacLean B, Cabolis K, Abeysiri S, Khong A, Sajic M, et al. The misogyny of iron deficiency. Anaesthesia. 2021;76 Suppl 4:56-62.
4. Stoffel NU, Zeder C, Brittenham GM, Moretti D, Zimmermann MB. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica. 2020;105(5):1232-9.
5. LaVallee C, Cronin P, Bansal I, Kwong WJ, Boccia R. Importance of Initial Complete Parenteral Iron Repletion on Hemoglobin Level Normalization and Health Care Resource Utilization: A Retrospective Analysis. Pharmacotherapy. 2019;39(10):983-93.
About the author:
 Assoc. Professor Chris Barnes
Assoc. Professor Chris Barnes
MBBS FRACP FRCPA
Lab: Clayton
Speciality: Haematology
Areas of Interest: Paediatric haematology, non–malignant haematological conditions including thrombosis and bleeding disorders
Phone: (03) 9538 6777
Email: chris.barnes@clinicallabs.com.au
Associate Professor Chris Barnes is the National Director of Haematology and provides strategic direction nationally for haematology at Clinical Labs. He is a clinical and laboratory trained haematologist who has been part of Melbourne Haematology and has worked with Clinical Labs (and previously Healthscope) for several years. A/Prof Barnes also works at the Royal Children’s Hospital and is director of the Haemophilia Treatment Centre. He has experience in both management and leadership positions. A/Prof Barnes has an active clinical research interest and is also director of Melbourne Haematology (Clinical) and Melbourne Paediatric Specialists.
Local pathologist near you:

Dr Shao Yang Tneh
BMedSc(Hons) FRACP FRCPA
Lab: Subiaco
Speciality: Haematology
Areas of Interest: Malignant and general haematology
Phone: 1300 367 674
Email: shao.tneh@clinicallabs.com.au
Dr Shao Yang Tneh is a dual trained clinical and laboratory Haematologist. He graduated from the University of Queensland in 2010 and underwent his basic physician and specialist haematology training in Queensland, rotating through the Royal Brisbane and Women’s Hospital, Gold Coast University Hospital, Mater Hospital Brisbane, Queensland Children’s Hospital and Australian Red Cross Lifeblood. He is a fellow of the Royal Australasian College of Physicians and the Royal College of Pathologists of Australasia. Shao was awarded the WA Cancer and Palliative Care Network Fellowship to undertake research at the Royal Perth Hospital in collaboration with the University of Western Australia. He has a research interest in translation haematology, which involves exploring new diagnostic methods for application in clinical practice. Shao holds an academic title as a Clinical Senior Lecturer with the University of Western Australia Medical School for his active involvement with education and training of medical students and junior doctors.